In my opinion, the run form is properly written, includes necessary information expected, and could very well be the report written for Michael. However, it could also be written by a paramedic (because it is clearly written by someone who understands how to write an ALS runform) who just happened to have an excessive amount of truthful information about the call. Therefore, I believe that it is most likely real.
I am now going to go through it. I do want to mention that someone of this will sound redundant to Dr. Jones' review. However, that is only because she did a pretty damn good job at going through it, and there's not much else for me to say in some instances. I will try to address other commonly asked questions or said statements about the run form. So here it is:

This is an F-902M form, which is the run form that is used by the LAFD. Since then, they have switched to using ePCRs which means they do not do paper run forms, everything is done on a computer.
Top left corner you will note "December 2004". No, this is NOT when this document was written. That is the date the run form layout was created. There are many documents that have a date similar to this or it may say "Dec 04" "12/04" "Rev. 12/04" or anything along those lines.
Everything in the Incident Info section is just that. Information about the incident. It includes the date, the incident number (which is unique to station 71), times, the pickup address, and the paramedics who were involved in his care and their employee numbers. These numbers are not their license numbers.
Keep in mind that we do not have scales in our ambulances and we do not weigh patients. When we write in a weight, if the patient cannot tell us their weight, we guess an approximate weight.
Next is Patient Information. Again, this is just that - Information about the patient. You have the patient's name, address, and date of birth. Yes, I do realize that they spelled Michael Micheal and the birth date is 8-28-58. Medics are not perfect. Spelling mistakes and numerical errors happen. There is no spell check button on paper to correct Micheal to Michael. And in the chaos of a code, even as smoothly as they run, you have a lot of work to do besides concentrating on the exact date of birth. In a code situation, I really only care about their age or at most, the year they were born. And even if I have the birth date, errors happen. My insurance carrier had my birth date a day early for like 2 years until I switched insurances. It happens. It's not like they're saying the patient is Joseph Jackson and his birth date is 2-28-1948.
The long number at the end is the patient file number assigned to the patient by UCLA.
Next we have the Comments section. This is where the medic wrote his narrative. Everyone writes their narratives differently. I use a modified SOAP form. Some medics use chronological. Others use strict SOAP. Some use some other fun way. It's all preference. Sometimes a medical director has a specific way they want a medic to write, but unfortunately, this is rarely strictly followed. So here is the narrative typed out for you. If something is written in parenthesis, it's a note I've added in:
"50 y/o male (they used the symbol for male) found supine on floor, CPR in progress, via PMD (Primary MD) Murray CA #G01168, no visible new trauma, good lung sounds following intubation, IV in place via PMD Murray Lt (left) leg, latter (thinking he meant “later”) IV Jug/Lt side (jugular on left side) via PM #1 (paramedic number 1 as listed above), pulses (they used the symbol for with) CPR, capnography initial 16 @ transfer 26, good lung sounds throughout and @ transfer."
Ok, so let's go through this. They found a 50 year old male lying on his back on the floor with CPR being performed by Mr. Murray. I honestly have no idea where they got the license number. I don't know if Murray told them a different one or what. They saw no trauma. They intubuated the patient and confirmed good lung sounds to say the tube is not in the belly. When they say lung sounds, they do not mean the physiological act of breathing. They mean that when the BVM is squeezed, you can hear air entering the lungs. If you didn't hear air, then you would assume the tube is in the belly, pull it out, and try again. An IV was placed by Murray in the left leg, and the paramedic placed an IV in the left jugular vein (in the neck). Now, it says pulses with CPR. Pulses WITH CPR. This doesn't mean the patient's heart is beating and he has a pulse, this means that they are getting a pulse with compressions, which helps to note they were doing good compressions. When you go compressions, you are doing the work of the heart and you are circulating blood. Therefore, you will be able to feel a pulse with compressions. The capnography is the end tidal, which is super confusing so I'm not going to get that far into it. However, the numbers there (from 16mmHg to 26mmHg) indicate he had been not been expelling as much CO2 when he was initially intubated as compared to after he had been ventilated and was brought to the hospital. This entirely normal. Finally, it notes that there were good lung sounds at transfer. This, again, does not mean the patient was breathing. They are just saying that the tube has not been dislodged at turnover, so if the tube gets pulled at some point, it wasn't with the paramedics because they were still getting good lung sounds at turnover to the ED. Phew!
Next is his medications and allergies. You may note that it says on the run form "No Viagra type <24 hrs". That's pertinent for patients complaining of chest pain because we nitrate chest pain patients. Nitro can tank their pressure to dangerously low levels if the patient has taken Viagra recently. I think it's kinda funny their run form has that written on there. Not strange by any means, but I thought it was clever. Anyway, meds aren't out of the ordinary, and there's an allergy to what looks like Thorizine (Thorazine)? Thorazine is an old medication that was used for a slew of different things. It's hard to say what he might have taken it for to establish that he was allergic. I would not venture to say why he had taken it previously because I don't know when he took it, and there are many different reasons to have taken it.
The section to the right is for billing purposes.

I'm putting all of the vitals together although I know that they are two different pictures, so bear with me. I'm going to go in chronological order.
At 1229, the patient had no blood pressure, no pulse, and was not breathing. This is how they found the patient. At 1233, the patient was in PEA. PEA is Pulseless Electrical Activity. This mean the heart still has some organized electrical activity, but is not producing a pulse. PEA is a lethal heart rhythm.
The medic gives 1mg of Epi (epinephrine) at 1234 through the IV in the left leg with no change. He then gives 1mg Atropine at 1236 in the left leg with no change. He gives another mg of Epi at 1240 or 1241 (I can't tell if he changed the 0 to a 1) in the left leg with no change. Epi and Atropine are given 3-5 minutes apart. Some medics do Epi and Atropine together, others space them out. It's all personal preference.
From this point, everything that is happening is happening in the ambulance. At 1311, the patient is still pulseless and apneic, has a GCS of 3 (which means there is no eye movement, no body movement, and not speaking. This is the lowest GCS you can have), and the patient is in asystole. Another 1mg of Epi is given now through the EJ with no response. A minute later at 1312, the patient is still in asystole and is given 1mg Atropine through the EJ with no response. Finally, at 1313, the patient is still in asystole and is given 50mEq of sodium bicarb with no response. Bicarb is used for prolonged downtime. At this point, the patient is still clinically dead.
So, sounds like the EJ was placed by the medics once the decision was made to continue resuscitative measures and continue to the hospital. I'm basing this on the fact that all meds were give through the IV in the leg from 1234 to 1241. There is then a time gap and meds are given through the EJ at 1311.
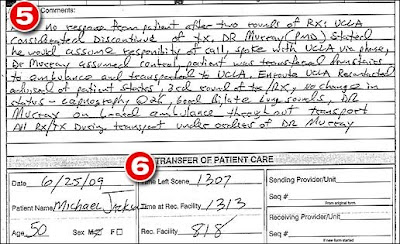
Then there is the Comments section. This explains what happened with Murray requesting continuation of resuscitative measures.
"(Unknown first word obviously due to it being blocked) no response from patient after two rounds of RX: UCLA considerated (considered?) discontinue of tx. Mr Murray (PMD) stated he would assume responsibility of call, spoke with UCLA via phone, Dr Murray assumed control, patient was transferred downstairs to ambulance and transported to UCLA. En route UCLA recontacted advised of patient status, 3rd round of tx/rx, no change in status - capnography @ 26, good bilate (bilateral meaning both lungs) lung sounds, Dr Murray on board ambulance throughout transport. All RX/TX during transport under orders of Dr Murray"
So, the patient received two rounds of ACLS medications with no change. UCLA was contacted to discontinue treatment. Then it's all plain English and pretty common sense. Finally, they called in to patch (radio into the hospital to let them know our ETA and what we've got), and it goes over the patient condition again.

Finally, this is the EKG strip that is being shown along with the report. The medics were using a Lifepak 12 monitor, and this is the printout of a Lifepak 12. The top two lines are the heart (EKG) and the bottom is the end tidal. The EKG to me looks like compressions and then stopping compressions to show asystole. The squiggly up and down you see is the result of compressions being performed. You then see asystole, which is the flatline. This is when the person performing compressions stopped so you could see the underlying rhythm, which is asystole.
The bottom line shows the end tidal. You can see that there are long boxes that rise above slightly. This helps to show the the ET tube is placed in the lungs and not in the esophagus. The waveform looks entirely normal for someone being ventilated.
Now, the time on the monitor says 1151. You have to manually set the time on the monitors. You have to set a watch, you have to set the time in your car, you have to set your microwave, you have to set your alarm clock, and you have to set these monitors. It is very possible that the monitor time had not been changed from day light savings time, and it was actually 1251.
So there you have it. My explanation of the Paramedic's Report. I tried to stay entirely unbiased and just explain things from a strictly medical standpoint. When I didn't, it was because of my experience as a paramedic. I hope I helped and feel free to post any questions you may have :)


